Living with back pain can be miserable, but unfortunately a surprisingly high number of people do. Approximately 65 million Americans have experienced or are currently experiencing back pain. Of that number, 16 million adults suffer from chronic back pain. It is a true pandemic of suffering.
Living with back pain can be miserable, but unfortunately a surprisingly high number of people do. Approximately 65 million Americans have experienced or are currently experiencing back pain. Of that number, 16 million adults suffer from chronic back pain. It is a true pandemic of suffering.
One of the most common causes of recurrent or chronic back pain is disc bulges, herniations, or disc degeneration. There is a non-surgical spinal decompression option that works in nearly 80% of cases but many patients elect to roll the dice with surgery. This is puzzling given the dismal facts surrounding surgery.
Studies show that lumbar fusion succeeds in barely 40% of patients. While that is a poor success rate, it gets worse. It seems “success” is a vague term.
In a study two years after spinal fusion was performed in “successful” procedures, pain was barely reduced by half for patients. To top it off, after surgery most of them continued using painkillers. This doesn’t sound like success to most people.
In another study, also two years after the procedure was performed, about 1/3 of patients reported that their pain was as bad as it had been before the operation. 14% believed that they were in worse shape after spinal fusion. Many will say that they would never do a lumbar fusion, but the minimally invasive procedures work great with few side effects, right? Not so fast.
There was a laser spine surgery craze in the mid-1990s that was touted as the answer to the problems of conventional surgery. It took more than a decade for a well-designed Cochrane Collaboration review to show that the minimally invasive group had a 38% revision rate, which is more than double of the group that underwent the standard procedure.
The American Journal of Medicine observed that in the United States about 80,000 spine surgeries fail annually. Patients who have not done well are referred to as “failed backs,” and they often return to the operating room repeatedly. In addition “failed backs” often lose ground after each procedure. About 1 in 5 patients who undergo spinal surgery for a degenerative disorder have to return for a revision procedure (a second operation).
Studies show that the second back surgery only has a 30% chance of success. This prognosis drops to 15% for the third back surgery and 5% for the fourth. Oregon Health and Science University spine medicine researcher Roger Chou believes that surgeons should be required to reveal the odds to their patients before going forward. “If [the surgeon] said, ‘Yes, we can do this $70,000 surgery. But you know, there’s still more than a 50% chance that you’re going to have a lot of pain, and you still won’t be able to work, and you’re going to need pain medicine, and you’ll have complications related to the surgery—and all this is well documented—then most people would say, ‘I don’t want it.’”
Tiger Woods, arguably the greatest professional golfer of all time, had a conventional microdiscectomy in 2014 and another in 2015. Both operations failed, leading to a third procedure in October 2015. Eight months later, Woods was downcast at a press conference. He did not know when or if he would play again. “I have no answer for that. Neither does my surgeon or my physio,” he said. “There is no timetable. There’s really nothing I can look forward to, nothing I can build toward.” He eventually had a fourth and fifth surgery.
Most orthopedic surgeons themselves don’t even want to have surgery. At an American Academy of Orthopedic Surgeons conference in the summer of 2010, a hundred surgeons were polled about whether they’d personally have lumbar spinal fusion surgery for unspecific low back pain. All but one answered, “absolutely not.” The risk-reward ratio just wasn’t good enough.
Non-Surgical Solution for Back Pain
So, what’s the non-surgical answer for reducing the suffering millions of Americans have with chronic low back pain? The answer is Vertebral Axial Decompression (VAX-D).
VAX-D is a revolutionary, non-invasive treatment for patients who suffer from low back pain, as well as leg pain and numbness caused from herniated or degenerated discs and posterior facet syndrome. Patients who have had back surgery—yet continue to experience low back pain and/or sciatica pain—may also be candidates for VAX-D.
How is VAX-D Performed?
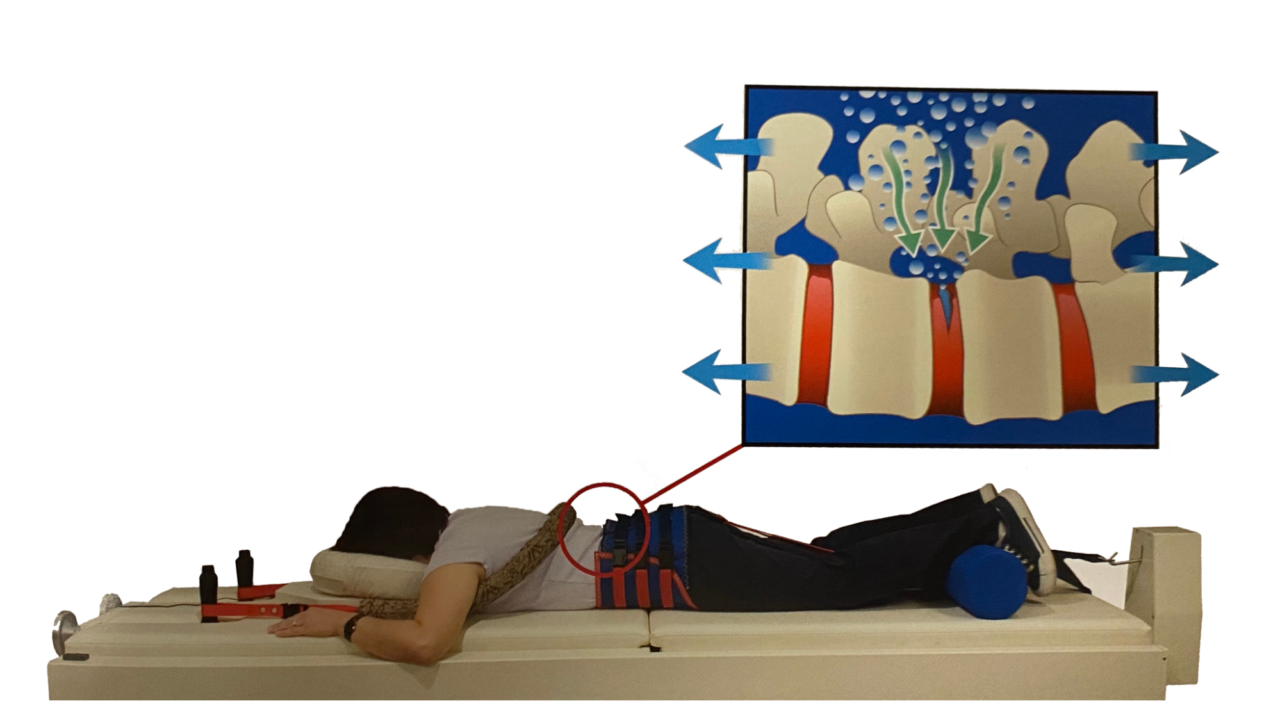
Prior to VAX-D treatment, patients are fitted with a patented ‘pelvic harness.’ They are then placed in a prone position on a VAX-D table and console (patients remain fully clothed during treatment). The VAX-D Therapeutic Table and Console technology applies and maintains a baseline tension of 20 to 24 pounds to the patient’s pelvis throughout the treatment session (even when at rest).
During treatment, patients utilize handgrips to extend the arms above the head (like hanging from a bar) to stabilize and restrain the upper body during lumbar distraction. The pneumatic-hydraulic cylinders of the Table are used to separate the lower table section from the upper section and apply tension to the patient’s pelvis. This creates a gentle pulling distraction of the spine off of the inflamed discs (called the decompression phase). There are 15 cycles of decompression with 15 cycles of rest between the decompressions for a total of 30 minutes per session.
A Negative is a Positive
 VAX-D is not like other treatments that only traction the spine and not offer decompression. Decompression means there is a negative pressure created in the disc, which causes diffusion of nutrients into the disc and a potential for healing of herniated or degenerative discs.
VAX-D is not like other treatments that only traction the spine and not offer decompression. Decompression means there is a negative pressure created in the disc, which causes diffusion of nutrients into the disc and a potential for healing of herniated or degenerative discs.
Whether you are standing, sitting or even lying down, there is a constant pressure down on the spinal discs. If the discs are worn, herniated or degenerating, more pressure is added on the discs, which creates greater pain. More pressure means more pain.
However, during the VAX-D treatment, negative pressure can be achieved. This creates a diffusion into the disc, a potential for a drawing back of herniated discs, and a rehydrating of degenerative discs.
VAX-D Successful Outcomes
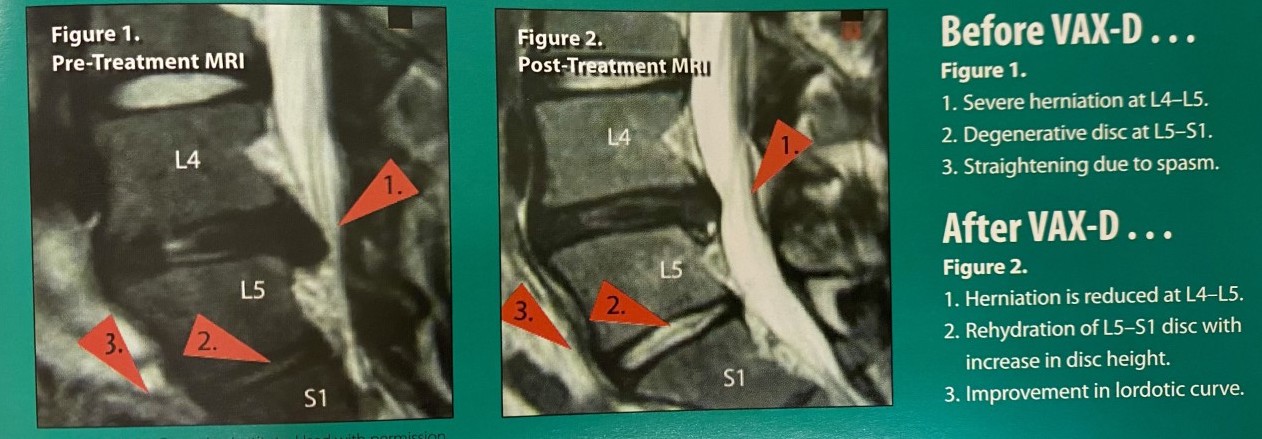 The photo above is a prime example of how VAX-D treatment can remove back pain. These MRI images showcase herniated and degenerative discs that caused significant pain for the patient. After VAX-D treatment, their spinal disc issues nearly resolved completely and their pain levels lowered significantly. These before and after MRI images give evidence of the possibility of herniated and degenerative discs being healed.
The photo above is a prime example of how VAX-D treatment can remove back pain. These MRI images showcase herniated and degenerative discs that caused significant pain for the patient. After VAX-D treatment, their spinal disc issues nearly resolved completely and their pain levels lowered significantly. These before and after MRI images give evidence of the possibility of herniated and degenerative discs being healed.
Imagine the reduction in back pain, morning stiffness, and sciatic pain in the legs the patient can experience after their VAX-D treatment. Based on the outcome of the example above, back pain relief is possible without having to undergo surgery.
Imagine you have tried conservative treatments for your back pain such as chiropractic care and physical therapy with no improvement. Maybe you have tried even more invasive procedures such as spinal injections or surgery with no help. Now imagine being referred to a hospital for surgery as your last option for relief. These are the type of patients that were referred to the Rio Grand Hospital in Texas for surgical consultations. Many of them were the worst of the worst and had exhausted their options.
However, the doctors prescribed 20 sessions of daily VAX-D treatment rather than surgery. A study published in the Journal of Progress in Neurosurgery, Neurology and Neurosciences concluded that out of 778 VAX-D treatments, 73% of the patients reported a successful outcome! As mentioned earlier, it is important to note what a “successful outcome” means. In this case, the successful outcome meant they reduced their pain to a 0 or 1 on a scale of 5. They also increased their mobility and their activities of daily living.
Team Care Method
At Team Health Care Clinic in Champlin, Minnesota, we have observed an even better outcome because we enlist our team of providers to address each patient’s unique needs. The Team includes medical nurse practitioners, physical therapists, chiropractors, acupuncture, massage therapy, and more.
Team Health Care Clinic has been the wellness clinic of choice for 30 years for many in the northern suburbs of the Twin Cities. In fact, Team Health Care Clinic was the first clinic to introduce non-surgical spinal decompression to the five-state region.
Counterfeit Decompression
Throughout the years, other providers observed the benefit of VAX-D and sought less expensive and less researched options for non-surgical decompression. We welcome others to come on board the mission of reducing back and sciatic pain with non-surgical options, however, it is important to ask the provider if they perform traction or decompression.
 Traction does not achieve negative pressure in the disc (see pictures above). Only decompression can create the negative pressure required to have a diffusion gradient into the disc.
Traction does not achieve negative pressure in the disc (see pictures above). Only decompression can create the negative pressure required to have a diffusion gradient into the disc.
Some providers are not even aware that the unit they purchased doesn’t have its own published studies, verifying that negative pressure needs to be achieved. Some manufacturers—when pressed for research—can only provide the published research of VAX-D and not their own.
Help For You
VAX-D helps to discover the root cause of the issue and directly resolves the back pain. Rather than going in with guesswork of what will relieve the symptoms, VAX-D works to actively correct problems with the spine so back pain relief can be achieved.
Team Health Care Clinic was the very first clinic to introduce VAX-D, a non-surgical spinal decompression treatment, to the Minnesota area. Throughout the years, other chiropractors have seen the beneficial results and have adapted the VAX-D protocol to spare others from back surgery.
 If you are looking for a non-surgical option for your back and/or sciatic leg pain, schedule a consultation with one of our providers at Team Health Care Clinic.
If you are looking for a non-surgical option for your back and/or sciatic leg pain, schedule a consultation with one of our providers at Team Health Care Clinic.